These Are The Surprising Everyday Causes Of Hairline Psoriasis That I Was Unaware Of
Why aren't we talking about it more?


Celebrity news, beauty, fashion advice, and fascinating features, delivered straight to your inbox!
You are now subscribed
Your newsletter sign-up was successful
Over my life, I've experienced bouts of hormonal acne, enlarged pores and sensitivity. But one thing I've never had to manage is dryness of any kind; you see, I'm much more prone to excess oil than patches of sore or flaky skin. That is, until I (pretty randomly) developed hairline psoriasis around six months ago.
Psoriasis around the hairline and across the scalp is fairly common; according to The Psoriasis and Psoriatic Arthritis Alliance, approximately 1 out of 2 (50%) of all people with psoriasis have it on their scalp. So where does it come from, and how can it suddenly impact you at any age? As someone who developed it in their thirties, I was keen to speak to skin specialists to discover the answers and learn how to address it, quickly.
What does psoriasis around the hairline look like?
First, let's start with the symptoms. For me, it was difficult to determine what was going on as my psoriasis tends to present at the back of my hairline rather than around the front (although from time to time, I do have an itchy red ring there, but it's subtle). I first started experiencing itching and felt a little rough patch on my left side. Annoyingly, I couldn't see this (even in a mirror) as it was in an awkward position and partially covered by hair. I only discovered it was psoriasis after asking a friend and my facialist to look at it.
Psoriasis is actually frequently mistaken for dandruff (seborrheic dermatitis) or eczema, so diagnosis depends on knowing the difference. To look at, psoriasis patches tend to be red and feel rough and itchy. "Psoriasis is well-demarcated," adds Dr Alexis Granite, a consultant dermatologist. "You can trace exactly where a plaque starts and stops with a lip liner." In contrast, "eczema tends to be fuzzy and hazy at the edges."
The subtle colour differences between psoriasis and eczema are also notable, says Granite. "Psoriasis scales are micaceous - silvery and flaky, like tiny shards of mica. Eczema scales are usually thinner and can look yellowish or greasy."
Another way to notice it? "Psoriasis is often asymmetrical, so if it's happening on one of any body parts, it will almost always be happening on the other side," explains Pamela Marshall, clinical aesthetician and founder of Mortar & Milk. Mine started on one side of my neck, but now presents on both sides.
Why does it occur?
One of my biggest questions I had was why I was getting psoriasis flare-ups in the first place. Because I have no history of eczema or dryness, it felt like it had come out of nowhere.
Celebrity news, beauty, fashion advice, and fascinating features, delivered straight to your inbox!
Psoriasis is actually a chronic immune-mediated, inflammatory condition, says Dr Granite. "Essentially, your immune system is over-communicating, telling your skin cells to regenerate at a frantic pace. While healthy skin takes about 28 days to cycle, psoriatic skin cycles in three to four days. These cells reach the surface before they are mature, piling up into the thick, silvery patches we call plaques." This overactive immune system can be caused by genetic factors or environmental triggers.
The hairline in particular is sensitive to psoriasis, as it's considered a 'transition zone.' "It’s prone to the Koebner Phenomenon, where the skin responds to even minor friction, from a headband, a tight ponytail, or even aggressive brushing, by producing a new plaque," notes Granite.
Marshall adds that the products we use can be major contributing factors in this area, too, mentioning "shampoos and conditioners with ingredients that our skin can't tolerate," in particular, with sulphates being a common culprit.
"It also can be due to not shampooing and conditioning your hair fully," she adds. "The hair really needs a double shampoo, a proper rinse, and then conditioner. So many people are worried about putting conditioner on their scalp because it might make their hair greasy. This is often avoided with a double shampoo. A single shampoo rarely removes all the dirt and grime. The scalp is also skin, and skin needs hydration. Without hydration, it panics."
Can you treat it from home?
When I experienced hormonal acne last year, I tried my hardest to treat it myself. But seeking professional help via a dermatologist was a game-changer for me, and allowed me to heal my skin properly. So, can you treat psoriasis from home? Largely, it depends on the severity and how long you've been trying.
If the problem is new and fairly mild, there are initial steps you can take. This starts with a comprehensive skincare routine, says Granite. "Regular use of thick, fragrance-free emollients helps reduce dryness, scaling and itch and supports the skin barrier," she begins. "Look for ointments or creams containing ingredients like petrolatum, ceramides, glycerin or urea."
She continues: "Gentle cleansing and avoiding harsh soaps or over-exfoliation are important, as irritation can trigger flares." Avoid strong shampoos (it may be worth going sulphate-free for a while, for example) and alcohol-heavy products.
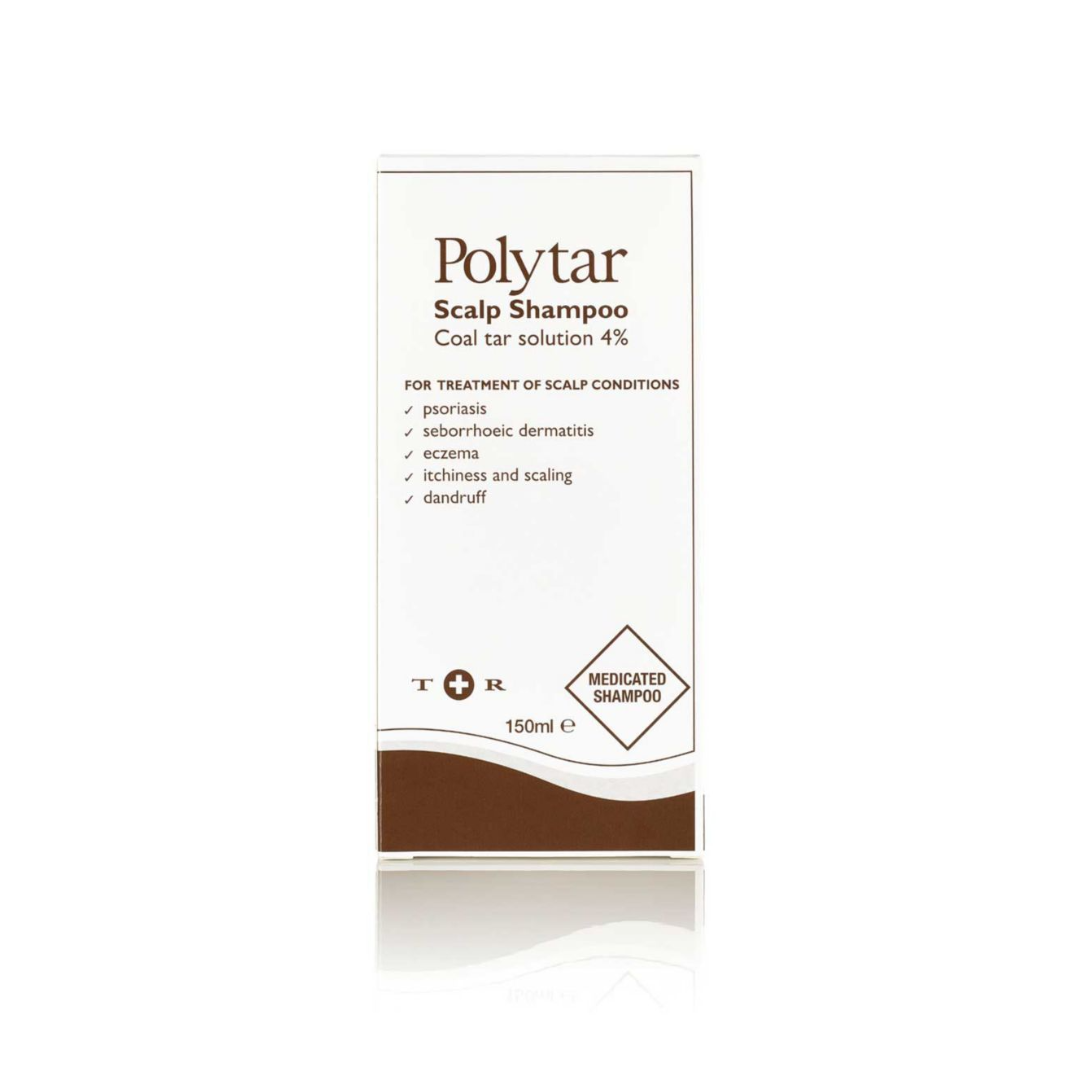
Marshall recommends trying gentle PHAs and plenty of Clinisoothe on the affected area, and Granite suggests salicylic acid for the scalp, as well as trying coal tar preparations (e.g. in certain shampoos), which can "reduce scaling and inflammation." LED light therapy (such as certain at-home masks) is also worth trying.
As stress is a common trigger, certain lifestyle shifts can also help manage symptoms. "Adequate sleep, regular exercise and avoiding smoking can all help reduce flare frequency," says Granite, with Marshall adding that taking probiotics can reduce inflammation in the gut.
At what point do you need to seek professional support?
Dr Granite says that any of the following are reasons to seek dermatologist aid: persistent or worsening symptoms (despite over-the-counter treatments), psoriasis covering larger areas of the body or affecting sensitive areas like the face, genitals, hands or feet, symptoms that are significantly itchy, painful or impacting sleep or quality of life, or any that are associated with joint pain or stiffness, which may suggest psoriatic arthritis.
"For moderate to severe psoriasis, prescription treatments are often needed," she explains. "These may include topical steroids, vitamin D analogues, non-steroidal anti-inflammatory topicals, phototherapy or, in more severe cases, systemic or biologic medications that target the underlying immune pathways."
In short, seeking dermatological help for skin problems like this is always recommended if you feel you cannot manage the problem alone.

Rebecca is a freelance beauty journalist and contributor to Marie Claire. She has written for titles including Refinery29, The Independent, Grazia, Coveteur, Dazed, Stylist, and Glamour. She is also a brand consultant and has worked with the likes of The Inkey List on campaign messaging and branded copy. She’s obsessed with skincare, nail art and fragrance, and outside of beauty, Rebecca likes to travel, watch true crime docs, pet sausage dogs and drink coffee. Rebecca is also passionate about American politics and mental health awareness.